Looking to the Future of Workers' Compensation

Several members of the PCG Health team recently attended the Workers Compensation Research Institute’s Annual Issues & Research Conference in Boston. The conference convenes researchers, regulators, and other workers’ compensation professionals from around the country to discuss trends they are seeing within the industry.
Below we share a couple of highlights from this year’s conference, including discussion about the future of the workforce and the movement of workers’ compensation insurance to value-based care. As always, if you have questions about these issues or want more information, we welcome you to be in touch by contacting Coy Jones at coyjones@pcgus.com.
Future Labor Force
Issues of workforce are inextricably tied to health care in the United States via employer-based insurance, the impact of unemployment on public health care programs, and the role of workers’ compensation insurance as a payor for health care services. This year’s conference on issues and research related to workers’ compensation opened with an analysis of our labor market today and trends as we look toward the future.
Dr. Erica Groshen, former Commissioner of the U.S. Bureau of Labor Statistics, opened the conference, by addressing the following questions:
- Is the economy as tight as a 4% unemployment rate suggests?
- How are artificial intelligence, robots, driverless cars, gig work, and more-fissured workplaces changing work as we know it?
- Should we trust and support official labor statistics in the era of big data and “fake news”?
Current labor market conditions: Since the end of the Great Recession, the U.S. has added 9.3 million jobs. As expected, the service industry has seen the most labor growth over the last year, particularly in the areas of professional services, leisure, and health services.
The unemployment rate is now down to 4.1%. Underutilization – discouraged workers, marginally attached workers, and involuntary part time workers – is also in decline. Of the unemployed population, 20.7% are long-term unemployed. As further proof of the tightening of the labor market, currently for every job opening, there is 1.1 unemployed person, which is comparable to the figures prior to the Great Recession.
Dr. Groshen also explored the relationship between productivity and wages. She expressed concern that, until 1973, wages and productivity tracked on a one-to-one basis, but, since then, productivity has soared and wages have been stagnant.
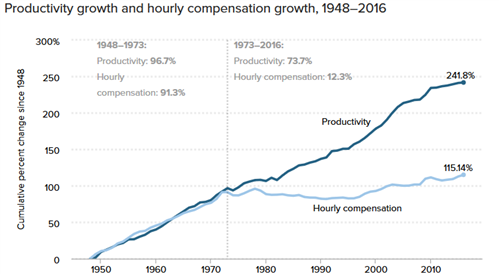
SOURCE: EPI analysis of Bureau of Labor Statistics and Bureau of Economic Analysis data
Dr. Groshen then turned to exploring the implications of key changes to our workforce.
Future of work: “Gig jobs,” defined as alternative work arrangements and/or contingent work, are on the rise, and Dr. Groshen pointed to concerns related to that sort of work. Gig jobs transfer risks from employers to workers. There is weaker employer responsibility to protect workers (health and safety, wage and hours rules, etc.), less stability for workers and communities (variable jobs or hours, less unemployment insurance, etc.), and less employer-provided training. The Bureau of Labor Statistics (BLS) Current Population Survey, however, has found that there does not seem to be any effect from what everyone perceives as a major shift in work and employment due to the emergence of the gig economy. There is some evidence though that people are not thinking about work for which they receive 1099 forms as ”jobs.” Dr. Groshen suggested that cognitive research is needed to figure out how people are thinking about gig jobs so BLS can adjust its tools and ask better questions.
Artificial Intelligence (AI): AI, which “replicates routine brainwork,” is also on the rise in the economy. When AI is applied to routine work, such as coding, the result is higher quality work done by fewer people who can focus on the complex tasks that only humans can do. As AI rises in society, many jobs will be lost, but other jobs will be created – similar to what happened when the economy moved from agricultural-based to industrial. Producing the new jobs will take time and displaced workers may lose one to four years of income. This will require government policy changes to help bridge the gap in employment.
Dr. Groshen concluded her session by emphasizing the importance of official statistics. Federal statistical agencies have experienced multiple budget freezes and cuts recently, even as the demand for better data has grown. It is a classic public goods problem. Everybody uses it, it would be undersupplied by the private market, but few people are ensuring that it continues to exist.
Workers’ Comp Moves Toward Value-Based Care
As in the rest of health care, the use of Value-Based Care (VBC) is growing in workers’ compensation insurance delivery systems. However, also similar to health care delivery more broadly, the acceptance of and readiness for VBC takes time. Also at the Workers Compensation Research Institute Annual Issues & Research Conference, Dr. Randall Lea presented findings from a recent, not yet published study that explored provider, payor, and regulator readiness to use value-based care delivery and payment models in workers’ compensation.
According to the study, most providers are informed about, interested in, and open to VBC – but not necessarily excited about the opportunity. Only one of seven providers surveyed is involved in some VBC activity through a limited one-payor pilot. That provider is positive about the experience but it is too early to evaluate the results.
The study found that payors are equally neutral about VBC opportunities. Only one of the seven payors surveyed is formally engaged in VBC (bundled payments). According to the study, payors prefer to focus on what they see as value and quality of care (e.g. high performing networks) and wait to see if VBC will “catch on” and be sustainable.
Most regulators surveyed are interested in VBC but cautious. One of the of the fifteen regulators in the study is doing work related to VBC and planning to expand those efforts. While other regulators are preparing for VBC, half of those in the survey are neither using VBC nor preparing for it, citing that they doubt “it will go in that direction.”
Despite the cautious attitude, the survey found that there are a number of providers, payors, and regulators that are currently engaged in conservative VBC. While they may not be ready to take on more comprehensive VBC models, they are implementing VBC fundamentals including pay for performance incentives.
Looking toward the future, the study outlined key considerations for those who would like to see VBC progress from idea to reality in the context of workers’ compensation insurance:
- Since policy change is not easy, VBC systems should be developed to work within the current rules.
- Providers need enough patients to make VBC work – providers will not be interested in risk-taking if there are not enough cases to spread the risk. Minimum number of cases might be difficult to guarantee in states where there is no or limited employer direction to specific providers.
- Because workers’ compensation benefits work differently than health insurance benefits, VBC in this context needs to implemented with a broader set of measures. Benefits are paid only if the injury was causally related to work, the patient is unable to work, and when residual impairment is ratable. Factors related to causation, Return To Work (RTW), and impairment need to be included in the VBC for workers’ compensation model.
- Survey participants recommended that guidelines for the adoption of VBC be developed:
- Good performing providers should be rewarded through financial incentives for participation, outcomes, and treating high acuity patients.
- There must be transparency across all stakeholders
- Payment models should be outcomes-focused, not discount-driven
- Models should be adaptable to current programs and regulatory conditions
- Reimbursement of providers should be fair and quick
- Reimbursement should be based on guidelines and compliance with medical treatment guidelines
- Fee schedules should not be used
- Patients should be steered to providers participating in VBC
- There should be a tight definition of outcomes and specificity around workers’ comp-related issues like RTW