Keeping a Pulse on Providers
While the medical well-being and cost benefits of home and community-based services (HCBS) are undeniable, the success of these programs is furthered when states implement technology-driven provider oversight approaches, like Electronic Visit Verification (EVV) systems, that help ensure accurate service delivery and claim submissions.
The passage of the 21st Century Cures Act, which requires all states to implement EVV systems for Medicaid-funded personal care services and home health service providers, makes consideration of EVV systems even more pressing.
More Than an Electronic Timesheet
Implementing an EVV system should provide you with more than an electronic timesheet. CareifyTM engages with each of these steps within a state’s HCBS program to help ensure appropriate care, accurate service delivery, and valid claims for billing.
- Collection of Prior Authorizations, Service Limits, and Eligibility
- Documentation and Validation of Service Authorizations
- Verification of Provider Services
- Claims Adjudication
- Program Monitoring and Reporting
State-Reported Savings
Please see below for state-reported cost savings generated through an EVV implementation.
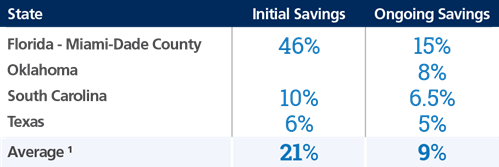
1 Reported by EVV Vendors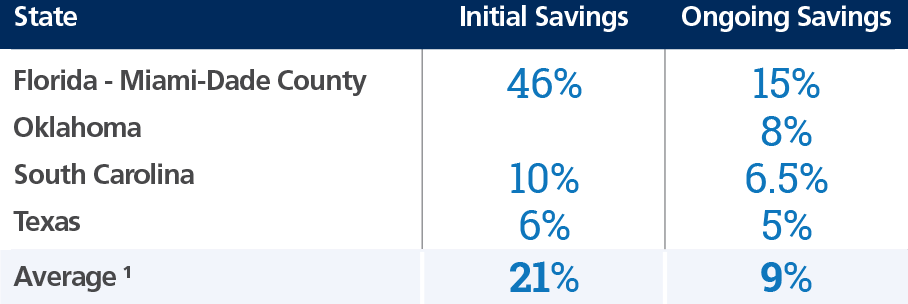
What About Third-Party EVV Data Aggregation?
Although the 21st Century Cures Act mandates certain functionality of EVV systems, the Act does not require states to utilize a single EVV system across all programs and agencies.
In response to this multi-system environment, PCG can provide a third-party EVV data aggregation system. This system collects provider visit information from any active EVV system in the state and validates that data against robust algorithms to check for program compliance and instances of fraud, waste and abuse.